15yr old female with anemia under evaluation
History taken by
Dr.Chandana Vishwanatham
Dr. Sai charan
Dr.Susmitha
15year old female who is the first child of a consanguinous married couple
her mother expired during the birth of 3rd child
She has 2 younger brothers who are apparently alright with no health related issues
Since childhood she has been having recurrent Respiratory tract infections(She almost always had cold,fever,cough with sputum) aggrevated during winters
Since 4yrs she is complaining of yellowish discoloration of eyes on and off not preceeded by fever with no h/o pruritus,No history s/o CLD
h/o easy fatigability , generalized weakness since 4years associated with loss of appetite,progressed to great extent in the last 2 to 3months
h/o short stature,failure to gain weight appropriate for her age and delay in secondary sexual characters
Attained menarche in 2020 October and now has 2months h/o of ammenohrea
4years back(2016) she had h/o jaundice and anemia for which one blood transfusion was done,her jaundice subsided slowly and she never had jaundice for the next 3yrs
2020 october she again developed yellowish discoloration of eyes which subsided on its own
2021 jan yellowish discoloration of eyes recurred and not subsided till now
h/o 2 blood transfusions in feb 2021
**************************************************
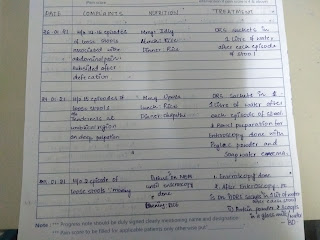
Evaluated in various hospitals since childhood
since the age of
2 years(9/2005),7.3kgs wt, started having fever,cold ,cough with expectoration,during which her x ray showed right middle lobe consolidation,hb 8.8,TLC,plts Normal,CRP strongly positive,smear for MP+
Diagnosis:Failure to thrive with recurrent RTI's
Treatment:cefuroxime drops and treated empirically with ATT(Rifampicin, isoniazid,pyrazinamide for 2months)
even after which she has been having recurrent cold, cough and high grade fevers
23/3/2006:LRTI ,CSOM diagnosed and treated
22/8/2006:B/L bronchopenumonia treated with syp.cefpodoxime
11/09/2006:cough,cold,fever
13/9/2006(Age 3yrs):Monteux test was done :positive with Erythema 12mm,induration 12mm and was started on ATT again for 2months
Hb 10.8,Tlc ,plts normal
AEC 408
4/1/2007(age 4yrs ,Wt 10.5kgs):Her symptoms did not resolve and continued with ATT for 4more months
15/6/2007:cold,cough,fever (102F)returned
also gave history of itchy lesions over hands and was diagnosed with Scabies and treated with ivermectin,permite cream
20/10/2007:Acute LRTI treated with antibiotics
27/05/2009and 11/07/2009:acute LRTI treated with antibiotics
7/9/2009:Hb 8.5,RBC 3million,AEC 476,
11/11/2010:LRTI
6/4/2011(Age 8yrs,Wt 11kgs) :LRTI treated with Iv antibiotics and inj deriphylline
serum ADA 10(normal <30)
12/10/2011:CT chest:Few prominent bronchi left lower lobe,B/L ground glass opacities
USG :Borderline spleenomegaly
10/12/2011 :LRTI
14/10/2011: Recurrent RTI,Failure to thrive, Protein energy malnutrition
Their differentials were 1.PEM with kochs,2.PEM with bronchiolitis,3.PEM with ?Enteric fever,4PEM with ARI/Hyperactive airway disease
Hb 10.8,WBC , platelets normal,MCV 68,McH 20.5,MCHC 30.5
serology negative
RFT,SGPT,ALP normal
2012 to 2014:5episodes of LRTI (Fever,cold,cough with sputum)
age 9yrs wt 13kgs
age 11yrs wt 16kgs
2/10/2014:Was having lesions on sides of neck and was treated with Acyclovir for Herpes
11/4/2016**:For the first time along with fever,cold and cough pt developed yellowish discoloration of eyes
Hb :9.0,RBC:3.1,TLC and platelet normal
TB 2.1mg/dl
1PRBC transfusion was done
Treated as ?Viral hepatitis
5/07/2016:cough+,chest x ray:Interlobar effusion upper and middle lobe, prominent brinchivascular markings? Bronchitis
9/8/2016,11/10/2016:LRTI
12/03/2017(13yrs 23kgs):LRTI,chest x ray :B/L upper lobe consolidations,hb 10.2,CUE:pus cells 19-20,alb trac
15/8/2017,7/10/2017,18/10/2017: Recurrent LRTIs
31/10/2017:Hb 10.6,TLc platelet normal
*************************************************
13/11/2017
For the first she visited our Hospital with c/o cough since 10days,sputum,SOB grade 1
In the background of recurrent LRTI,2D echo was done
2D echo in our hospital showed Moderated SA VSD( left to right shunt),EF 68%,Good LV systolic function,trivial TR
hb 11,TLC 6200,plt 5lakhs
pt was immediately taken to cardiologist
2D echo at an outside corporate hospital:normal sized chambers,No RWMA,Normal LV/RV function,
nothing mentioned about VSD
so she came back to our hospital and was in follow up with dept of TB and chest for 2 yrs till the end of 2018 being treated for allergic brinchitis
She was prescribed with various medicines for her Recurrent LRTIs(symbecort inhalers,moteleukast,aphylline tabs,Tab ferreo XT etc) and nothing helped
8/7/2019 to October 2019(age 14yrs wt 24kgs): They stopped coming to our hospital and went to other local hospitals for RTIs
Human growth hormone was done:4.53ng/ml (which is normal)
USg moderate spleenomegaly
hb 8.1,TB 2.1mg/dl
30/5/2020:loss of appetite started and on and off pain abdomen(subsided later) upon her background of LRTI continued
16/08/2020 :Hb 8.1,RBC 3.7million,MCV 77,MCH 27.1,TB 3.9mg/dl
5/10/2020:Her yellowish discoloration of eyes recurred lasted for about 1 month and subsided on its own(TB 4.4mg/dl-->1.2)
18/1/2021:she again developed yellowish discoloration of eyes ,TB 3.9,direct 2.6,indirect 1.3, with mild spleenomegaly on USG
?Gilbert,? Hemolytic anemia
24/1/2021
upper GI endoscopy done:Normal
26/1/2021
Hb 5.6,RBC dropped to 1.2M***,MCV 141,MCH 36,Dimorphic picture shows macrocytic,normochromic ovalocytes ,tear drop cells and 7-8 rbcs/100wbcs
High performance liquid chromatography
HbA 87.4%
HbF 0.6%(<1 is normal)
HbA2 :3(normal 2-3.5)
serology negative
urine reactive for bile salts and bile pigments
Hb 6.0,RBC 1.9M,TB 3.1
**************************************************
She was taken to NIMS admitted under gastroenterology from 4/2/2021 to 13/2/2021
Hb 9.6
TLC plts normal
retic count 4%
retic index 1.85%
RFT normal
coombs DCT,ICT negative
thyroid function tests normal
ANA immunofluorescence negative
IgG TTG negative
anti endomyseal ab negative
G6PD 30.3 (normal)
LDH 544(raised)
Was prescribed with oral iron and B12 for 2weeks and she came back home
*************************************************
After 4days 17/2/2021 her generalized weakness,loss of appetite and jaundice has aggrevated for which she was admitted in local hospital where 2 blood transfusions were done
Before admission:Hb 6.5,TB 3.9,RBC 2M
At the time of discharge(20/2/2021)Hb 10.0,TB 2.2,RBC 4M
Total protein :6mg/dl
**************************************************
After 4days she was taken to a top govt hospital with drop in Hb again post transfusion (Hb 9.3,RBC 3M,plt 2L,DCT 3+)
1/3/2021 In osmania pt was adviced for vit B12 levels,folic acid levels,osmotic fragility test,serum ferritin,hb electrophoresis again
From ther they went to a top corporate hospital where pt was diagnosed with ?AIHA
adviced for clinical exome sequence,they gave the sample for sequencing ,it takes one month for the report(report awaited)
and was started on Tab Wysolone 20mg OD from march 1st 2021 and was asked to review after 2 weeks
but in the meanwhile pt and her attendors felt that her jaundice and her generalized weakness progressed suddenly and was brought to our hospital.
**************************************************
O/E pt short thin built,Wt 28kgs
gen exam:Pallor+,Icterus+,
No lymphadenopathy,pedal edema
JVP raised
RS:
chest expansion 1.5cms which appeared a little less on right side
dull note on percussion of Rt ISA,all other lung fields resonant
Auscultation:BAE+,?Bronchial BS rt ISA and decreased Air entry rt ISA
P/A
shape normal
umbilicus central , inverted
no increase in local temp,no tenderness
Mild spleenomegaly+
No hepatomegaly
BS+
No free fluid
Diagnosis:
Autoimmune hemolytic anemia
?Common variable immunodeficiency syndrome
Recurrent RTIs
Indirect hyperbilirubinemia
Failure to thrive
hb 3.2
tlc 8,200
plt 3.0l
RBC 0.8M**
MCV 116
MCH 37
MCHC 31
RDW 25(increased)
TB 8.16
DB 0.77
AST 43
Alt 23
ALP 113
Tp 5.9
Alb 4.6
A/G 3.4
narrow gamma gap is noted
RFT normal
PBS macrocytes,macroovalocytes,anisopoikilocytosis with hypochromia
coombs:
DCT 4+(positive)
ICT 1+
Auto control 3+(positive for auto antibody,thermal amplitude test awaited)
For 17/F
A 17 year old lady presented to the emergency room with jaundice since 2 days. She also reported exertional dyspnea, fatigue and pedal edema since 2 days.
Her past history was also significant for recurrent childhood lung, ear and sinus infections. She also has been having persistent anemia (chart in the blog) since early childhood. She also had significant developmental abnormalities with short stature (growth chart plotted in blog) and wasting (growth chart in blog) and also delayed menarche. Dietary history was insignificant and she did not have any bowel or bladder dysfunction.
Clinical examination from head to toe revealed a patient with short stature and in mild respiratory distress. Her vitals at presentation were -
PR - 150 BPM
BP - 100/60 mm Hg
Temp - 98.4 F (chart shared in the blog)
RR - 26/min
Spo2 - 98% on room air
GRBS - 130 mg/dl
The patient had severe conjunctival pallor and lemon yellow scleral icterus. She did not have any features of active sinusitis, tongue was pale and bald. No cervical, axillary or inguinal lymph nodes were not palpable. Skin turgor was normal and no rashes were observed.
Her nails were pale and showed Quincke's pulsations, consistent with high output state/failure. She also had cervical venous hum and prominent abdominal aortic pulsations. Examination of feet showed pitting type pedal edema extending upto her ankles.
Systemic examination was significant for hyperdynamic precordium, palpable P2 and raised JVP. Auscultaton revealed a loud P2 with a pansystolic murmur along the left sternal border accentuating on inspiration. She also had an S3 gallop, accentuating on inspiration. Auscultation of the right femoral artery with occlusion of forward flow revealed a diastolic bruit. Respiratory system exam was significant for decreased intensity of breath sounds. Abdomen exam showed moderate splenomegaly and mild hepatomegaly. CNS exam was insignificant.
After reviewing her past medical records and her current history and physical exam, she was diagnosed with Autoimmune Hemolytic Anemia with Acute High Output Heart Failure.


Comments
Post a Comment